Abstract
Introduction:Acute kidney injury (AKI) and chronic kidney disease (CKD) affect 10-70% of transplant recipients. Onset of kidney injury varies from days to months or years after transplantation. Kidney injury may be caused by multiple factors. Long-term data on cyclosporine induced nephrotoxicity post HSCT are limited. It is unclear if cyclosporine induced nephrotoxicity at early phase post HSCT will impact long term renal function. The objective of this study is to evaluate the progression of renal function in allogeneic hematopoietic stem cell transplant (HSCT) patients, before, during and after cyclosporine therapy.
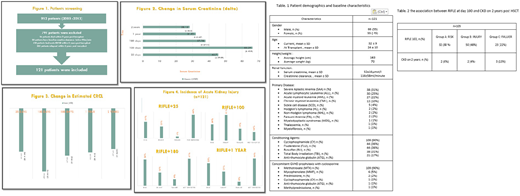
Methods:This is a retrospective single arm cohort study evaluating the impact of cyclosporine on renal function in patients who underwent allogeneic HSCT from 2003 through 2013. Patients age≥ 14 years who underwent allogeneic HSCT and received cyclosporine as graft-versus-host disease (GVHD) prophylaxis and alive two years post HSCT without disease relapse or GVHD were included in the study. Primary outcome was the change in serum creatinine and estimated creatinine clearance. Delta creatinine (baseline creatinine - creatinine on day 25, day 100, day 180, year 1 and year 2 post HSCT) was used to calculate the change in the serum creatinine and estimated creatinine clearance. Estimated creatinine clearance was calculated using Cockcroft and Gault formula (CG) for patients aged ≥ 18 years. Schwartz formula was used to estimate creatinine clearance for patients aged ≥ 14 years till 18 years. The secondary outcome was the incidence of acute kidney injury. AKI was defined as per RIFLE criteria. The severity grades were defined on the basis of the changes in serum creatinine. CKD was defined if estimated glomerular filtration rate (GFR) <60 ml/minute per 1.73 m2 for 3 months. All patient during the study period were screened. Descriptive statistics were used to describe the data, continuous variables were reported as mean ± stander deviation and categorical variables were summarized as frequencies and percentages. The study was approved by the Office of Research Affairs in our institution.
Results: Out of 912 patients who underwent allogeneic HSCT from 2003 to 2013, 121 patients were included who met the inclusion criteria listed above in the method section (Figure 1). The majority of patients were males (55%) with sever aplastic anemia as primary disease (31%). Mean baseline serum creatinine was 52±16 µmol/l, mean baseline estimated creatinine clearance was 116±58 ml/minute per 1.73 m2 (Table 1). Mean duration of cyclosporine levels monitoring was 232±180 days. Serum creatinine increased from the baseline at day 25, day 100, day 180, 1 year and 2 years post HSCT (Mean± SD; 45.7 ±39, 66.2 ±45.9, 37.8±27.1, 31.9±22.55, 28±22.5 µmol/l, respectively) (Figure 2). This translated into reductions in the estimated creatinine clearance at day 25, day 100, day 180, 1 year and 2 years post HSCT (Mean± SD; -61.6±51 , -89.6 ±55.7,-67. ±55.34,-62.5±55.4,-57.6±56.ml/minute per 1.73 m2, respectively) (Figure 3). The highest incidence of AKI was at day 100 post HSCT in the included patients. 40% of them had supratherapeutic cyclosporine levels. There was association between developing acute kidney injury at day 100 and CKD at 2 years post HSCT, 23% of the included patients had acute kidney injury and 13 % of them found to have CKD at 2 years post HSCT as illustrated table 2.
Conclusion:Our study demonstrated that cyclosporine represents a primary risk factor for progression of renal impairment in hematopoietic stem cell transplant recipients particularly in those who developed acute kindly injury at 100 days.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal